Stories > Mission To Transform Lives
Mission To Transform Lives
A collaborative Haemodialysis Care Project brings together healthcare professionals from Singapore and Vietnam to help raise standards of renal care in the region.
BY GOH HWEE KOON
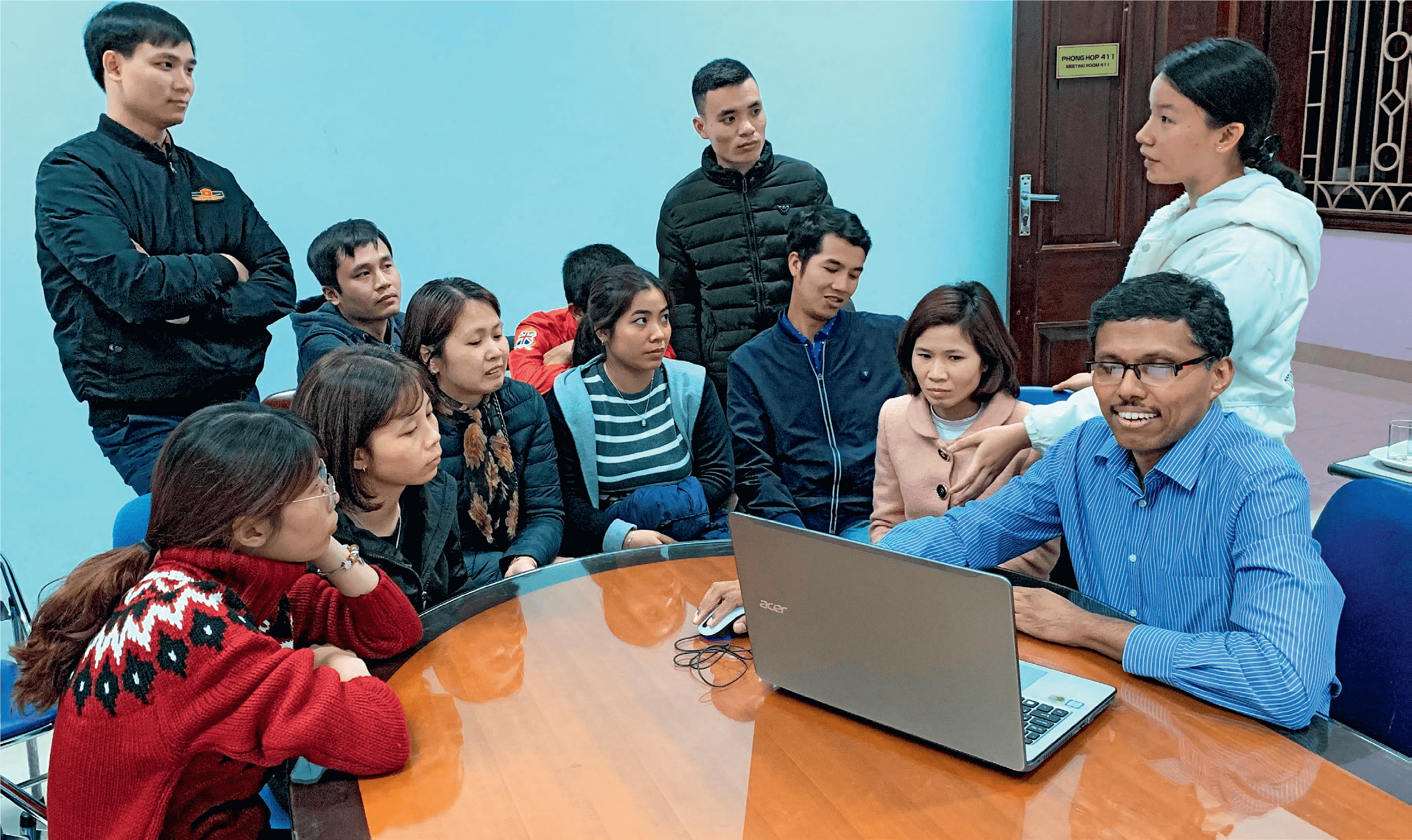
Dr Manohar Giliyar Bairy, alongside Vietnamese master trainers, shares his knowledge and expertise with haemodialysis care professionals in north Vietnam.
hen your kidney health deteriorates to the point of being unable to filter wastes and extra fluid from your blood, undergoing a treatment like haemodialysis becomes necessary. At least 2.9 million people in Asia need dialysis, according to a 2015 report from the National Library of Medicine.
Although a lifesaving therapy, dialysis is also an expensive treatment, which explains its limited use in countries with fewer resources in this field. Among the countries in Southeast Asia that have taken strides towards improving the standard of renal healthcare is Vietnam. In 2018, the Haemodialysis Care Project (HCP) was launched in northern Vietnam. The three-way collaboration involved Hanoi Medical University (HMU), Tan Tock Seng Hospital (TTSH), as well as the Singapore International Foundation (SIF), with Bach Mai Hospital and Viet Duc Hospital as the main participants.
The five-year initiative was focused on enhancing the training of haemodialysis caregivers to deliver safe treatments, and updating them on the current standards of care. Led by Dr Manohar Giliyar Bairy, a senior consultant in the renal medicine department at Singapore’s TTSH, the project aimed to build capacity within the healthcare system in Vietnam by grooming a group of master trainers, who would then cascade the training across north Vietnam.


Healthcare professionals in Vietnam’s haemodialysis sector have benefitted from the Haemodialysis Care Programme, through which they learnt the latest techniques in the field.
The main components of HCP included clinical training that covered modules on topics ranging from the principles of haemodialysis to management of complications and quality assurance, as well as leadership engagement sessions. One module included a study visit to Singapore to learn about the country’s standards of care and clinical practices, and a symposium where healthcare professionals from both countries shared current standards, the latest research, and public health collaterals in haemodialysis.
“We did not meet a single trainee or
Hanoi faculty in the programme who
was not passionate about enhancing
the standards of their practice, even
when resources were scarce.”
Dr Manohar Giliyar Bairy, Tan Tok Seng Hospital, Singapore
THE RIPPLE EFFECT
As the programme gained momentum,
Dr Manohar and his team did not just
find great satisfaction in sharing their
knowledge and expertise, but also
deep appreciation for the passion and
commitment of the participants.
“Healthcare workers could well turn cynical and jaded in resource-poor settings, and that would be understandable,” he explains. “But we did not meet a single trainee or Hanoi faculty in the programme who was not passionate about enhancing the standards of their practice, even when resources were scarce.”
By the time HCP ended its run in March this year, 12 Vietnamese master trainers had graduated from the programme. It is estimated that more than 230 Vietnamese haemodialysis care workers had honed their skills via cascade training, while 3,960 haemodialysis care workers and patients in northern Vietnam had benefited from it.
“Apart from the numbers, it is important to note that the local participants were able to change the culture of haemodialysis care practices such as on asepsis, catheter care and infection control in their hospitals — and hopefully amplify this effect in other centres in the region,” says Dr Manohar. “In healthcare, like in society, once the wheel of change is set in motion, it tends to gather momentum.”
One of the greatest improvements is in the area of catheter care. The procedure, which is used on patients who have trouble passing urine normally, involves using a hollow, partially flexible tube that collects urine from the bladder and leads to a drainage bag.
Just five years ago, only doctors in Vietnam could perform catheter care on, and monitoring of, haemodialysis patients. Today, however, even nurses are trained to perform catheter care work for haemodialysis patients.

“We are certain that the
friendships and spirit of
cooperation between our
communities will continue
for many years to come.”
Ha Phan Hai An, associate professor, Hanoi Medical University
MAKING A DIFFERENCE
Among the challenges that Dr
Manohar faced, the language
barrier was a big problem, as
English was not the medium of
instruction. But translators and
English-speaking students in
Hanoi managed to help overcome
this problem. “Additionally,
the resources available to our
trainees were not comparable
to Singapore. This required
improvisation and resilience in
finding solutions,” he adds.
“They were always responsive to our suggestions and took pains to develop training videos in the local language. When we learnt that they were vigorously disseminating the training across the province, the reach of the programme staggered us, albeit pleasantly.”
Although the HCP has ended, the door remains open for collaboration opportunities between Singapore and Vietnam. Moving forward, HMU is keen to explore sustainability plans that include a review of the hospitals’ internal standard operating procedures based on the guidelines currently being developed by the Vietnam Kidney Association, and continue digitalising training resources to achieve wider outreach.
There is also potential for a new nephrology project in Ho Chi Minh City, and a submission of a scientific paper based on the HCP project’s positive outcomes for publication in medical journals.
“We are pleased to have worked with the SIF and TTSH on this meaningful project,” says Hà Phan Hai An, associate professor, HMU. “We are grateful for the warm support from the Singapore International Volunteers, who have worked tirelessly to impart knowledge to Vietnamese trainees over the years.
“We are certain that the friendships and spirit of cooperation between our communities will continue for many years to come.”
HCP’S DEVELOPMENTAL IMPACT
INDIVIDUAL
A boost in the confidence
of nurses, due to having
gained new skills and
knowledge. All trainees
under five years of
service achieved a
100 per cent passing
rate last year and are
currently certified to
train their peers.
INSTITUTIONAL
INSTITUTIONAL
Internal training is
now conducted within
hospitals to share
knowledge among
nurses – to help create
standardised procedures
and develop curriculum
for new trainees.
SECTORAL
Master trainers now
have a mandate to
conduct training for
other institutes and
haemodialysis care
workers, as well as new
healthcare workers and
medical students. An
annual plan is also in
place for the continuous
training of medical staff.
SOCIETAL
Patients can now
receive catheter care
right after dialysis
without waiting for
doctors to be available.
Closer monitoring
and evaluation of new
patients, as well as long-term
management plans
for existing patients, are
also available.
